Non-alcoholic fatty liver disease (NAFLD): What you need to know
Non-alcoholic fatty liver disease (NAFLD) is a condition caused by a build-up of fat in your liver. It’s more common if you’re carrying excess weight or if you have certain health issues like type 2 diabetes. Left untreated, NAFLD can eventually progress to a stage called cirrhosis, where your liver becomes permanently damaged.
Making healthy lifestyle changes is one of the most effective ways to prevent NAFLD from progressing. If you have a BMI over 35 and a weight-related health condition, you may be eligible for NHS-funded support from Oviva. You’ll receive personalised care from healthcare professionals and could access prescription weight loss medication.
Key Takeaways:
- Non-alcoholic fatty liver disease is caused by a build-up of fat in your liver cells.
- Your risk of developing NAFLD is higher if you’re carrying excess weight or if you have conditions like type 2 diabetes and insulin resistance.
- NAFLD is unlikely to have symptoms in the early stages. Over time, it can advance to cause permanent liver damage and serious health issues.
- It’s essential to take steps to reverse NAFLD, including adopting a healthy, sustainable diet, exercising regularly and seeking professional support.
What is fatty liver disease (NAFLD)?
Non-alcoholic fatty liver disease (NAFLD) happens when too much fat builds up in the liver. This fat accumulation is called steatosis, and when it occurs in the liver, it marks the first stage of fatty liver disease.
As the name suggests, NAFLD isn’t caused by alcohol – it’s linked to other factors, often related to metabolism.
You might also hear NAFLD called metabolic dysfunction-associated steatotic liver disease (MASLD). This updated term reflects the condition’s connection to how the body processes and stores energy.
The four stages of NAFLD
NAFLD can progress over time, moving through four main stages:
1. Simple fatty liver (steatosis)
This is the first stage, where fat has built up in the liver cells – but there’s no inflammation or damage. Most people have no symptoms, and it’s often picked up incidentally during tests for other conditions.
2. NASH (non-alcoholic steatohepatitis)
In this second stage, the liver becomes inflamed, and cell damage may occur. It’s more serious than steatosis, but still reversible. Like the first stage, it can develop without symptoms.
3. Fibrosis
Ongoing inflammation begins to cause scarring in the liver. At this point, some liver damage has occurred, but with prompt lifestyle changes, it’s still possible to slow or even reverse much of the damage.
4. Cirrhosis
This is the most advanced stage, where extensive scarring causes the liver to shrink and lose function. At this point, the condition is irreversible and may lead to liver failure or cancer.

What causes fatty liver?
Your risk of non-alcoholic fatty liver disease is higher if you:
- Are carrying excess weight, especially around the abdomen
- Have insulin resistance
- Have type 2 diabetes
- Are over the age of 50
- Have high blood pressure
- Are a smoker
- Have an underactive thyroid
The most common cause of fat accumulation in the liver is carrying excess weight, usually from eating more calories than your body needs and/or leading a sedentary lifestyle.
Despite the name, fatty liver disease isn’t caused directly by eating fat. Research shows that refined carbohydrates are more strongly linked to fatty liver than dietary fats. Total calorie intake is a more significant risk factor.
Another key driver is insulin resistance – when your cells don’t respond properly to insulin, the hormone that helps regulate blood glucose. Insulin resistance is associated with type 2 diabetes and polycystic ovary syndrome (PCOS) and can be influenced by genetics, excess body weight, or a low-activity lifestyle.
Insulin resistance disrupts the way insulin regulates fat metabolism, leading to more free fatty acids (FFAs) being directed to the liver – contributing to fat build-up over time.

What I love about Oviva is that I can eat what I want — it was a completely new experience for me not to count calories. I lost 5 kg in the first 12 weeks, and my blood pressure normalised.
Fatty liver in women
Women may face unique risk factors when it comes to NAFLD. For example, the risk increases after the menopause, due to a higher likelihood of developing insulin resistance and a tendency to accumulate abdominal fat.
Another key factor is polycystic ovary syndrome (PCOS). PCOS can raise the risk of fatty liver because of associated weight gain and a strong link with insulin resistance.
Symptoms of fatty liver disease
In most cases, non-alcoholic fatty liver disease has no symptoms during the initial phase of simple steatosis of the liver.
As it advances, some of the possible fatty liver symptoms include:
- Fatigue
- Weakness
- Upper right abdominal pain
If it advances to the point of cirrhosis, you may experience:
- Jaundice (yellowing of the skin and whites of your eyes)
- Swelling in the legs, ankles, feet or stomach
Is fatty liver dangerous?
The early stage of fatty liver disease is usually harmless, but as it progresses into NASH, fibrosis, and cirrhosis, it becomes more serious – and can eventually be life-threatening.
That’s why it’s important to take action early and prevent the condition from advancing.
NAFLD can also raise your risk of heart disease and diabetes complications.

Can fatty liver be reversed?
Yes, non-alcoholic fatty liver disease (NAFLD) can be reversed – but only in the early stages. Once it progresses to cirrhosis, the damage becomes permanent. Some effects of fibrosis may also be irreversible, which is why it’s important to act early.
The excess fat in the liver can often be reduced through weight loss and lifestyle changes. If you’re eligible, personalised support from Oviva can help you achieve sustainable weight loss and make lasting improvements to your health and wellbeing.
How to treat and prevent NAFLD
You can take action to prevent non-alcoholic fatty liver disease (NAFLD) or stop it from progressing to more serious stages like fibrosis or cirrhosis. The key is to make healthy, sustainable lifestyle changes – focusing on weight loss, diet and overall wellbeing.
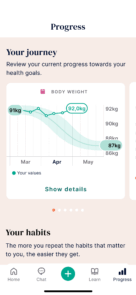
If you’re living with overweight or obesity, aim to lose around 7% of your body weight to reduce liver inflammation, and more than 10% to improve fibrosis. The National Institute for Health and Care Excellence (NICE) recommends aiming for 5 to 10% weight loss over six months.
There’s currently no targeted medication for NAFLD, but some related conditions can be treated – such as obesity with Wegovy, and type 2 diabetes with metformin.

Diet
Eat a nutritious, balanced diet with lean protein, fibre, and healthy fats.
NICE guidance recommends the Mediterranean diet, which focuses on:
- Fruits, vegetables, legumes and whole grains
- Fish, nuts and olive oil
- Moderate amounts of poultry and low-fat dairy
Research shows this diet can:
- Support weight loss
- Help with long-term weight management
- Reduce liver fat, even without weight loss
Try to limit sugar and processed foods. Small swaps – like choosing zero-sugar drinks and whole foods instead of takeaways – can make a big difference. Not sure where to start? Try our seven-day healthy weight loss plan.
If you have a condition like type 2 diabetes or PCOS, consider cutting down on refined carbs, such as white bread, white rice, and crisps, as these can spike blood glucose.
Try to reduce or avoid alcohol, as it can worsen liver damage and make weight loss harder.
If you snack in the evenings, focus on eating the right foods before bed.
Lifestyle
Start moving in a way that works for you – becoming more active can make a big difference to your liver health – but that doesn’t mean jumping straight into intense workouts.
It’s okay to start small. Even light movement, done consistently, can begin to improve how your body processes fat.
NICE recommends aiming for 150–200 minutes of moderate activity per week, but this might take time to build up to – walking for a few minutes, stretching, or doing seated exercises can all count as a starting point.
What matters most is finding ways to move regularly that feel achievable for you. As your energy increases and your confidence grows, you can build on this foundation over time.
And if you smoke, try to stop – it’s linked to worsening NAFLD and affecting insulin function.
If you want support building healthy weight loss habits, Oviva’s NHS-funded weight management programme can help. You’ll receive personalised care, and may be eligible for weight loss injections.
How long does it take to reverse NAFLD?
Reversing NAFLD is a gradual process. It may take several months to see meaningful improvements – especially if you’re aiming for 5 to 10% weight loss.
The most important part? Staying consistent with your healthier lifestyle to protect your liver long term.
Can you live a full life with NAFLD?
Yes – with early action and the right support, it’s possible to live a long and healthy life with NAFLD. The key is to focus on realistic, sustainable changes rather than short-term fixes or extreme diets that are hard to maintain.
Even if your condition has progressed, some liver damage may still be reversible, and you can take steps to improve your symptoms and overall wellbeing.
Take the next step with Oviva
Living with non-alcoholic fatty liver disease? You don’t have to face it alone. With the right support, it’s possible to reverse early-stage NAFLD and take back control of your health.
If you have a BMI over 35 and NAFLD, you may be eligible for professional support through Oviva’s NHS-funded programme. You’ll get tailored care from a team of doctors, dietitians and psychologists, with practical support to help you manage NAFLD.
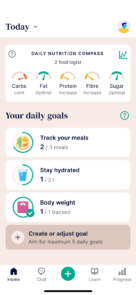
With Oviva’s weight management programme, you will:
- Make sustainable changes to your diet and lifestyle
- Chat directly with healthcare professionals for personalised support
- Track progress in the Oviva app, including meals, weight and habits
- Build long-term habits – no strict diets or quick fixes
- Access prescription weight loss injections (if appropriate)
97% of Oviva users recommend us and, on average, lose 13.6 kg in the first year.
It’s easy to find out if you’re eligible – just ask your GP!
Not sure how to start the conversation? That’s why we created our info pack – download it for everything you need to know.