Menopause, high blood pressure and HRT: here’s what you need to know
Menopause can increase your risk of high blood pressure (hypertension). And symptoms of high blood pressure, like headaches or fatigue, are often mistaken for menopause, so regular blood pressure checks are important.
Here, we’ll cover how to navigate your health with care through menopause, including when HRT is safe to use and how to manage high blood pressure.
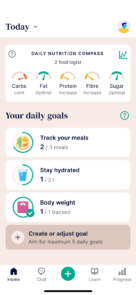
If you’re experiencing overweight or obesity, this can intensify menopausal symptoms (VMS) and raise your blood pressure. That’s where Oviva can help – our NHS-funded weight management includes personalised, expert support and the Oviva app where you can track your progress, including blood pressure.
Key Takeaways
- Menopause and perimenopause can increase your blood pressure, but factors like age and lifestyle play a role too.
- Blood pressure can fluctuate during menopause – one high reading doesn’t mean you have hypertension and tracking blood pressure over time is more accurate.
- It’s often possible to safely take hormone replacement therapy (HRT) if your hypertension is under control, especially using HRT patches and gels.
- Regular monitoring and lifestyle adjustments, like a balanced diet, regular exercise and weight management, can help you manage blood pressure during menopause.
Can menopause cause high blood pressure?
Yes – menopause can cause high blood pressure. There’s a few reasons why:
- When your periods stop (perimenopause), hormonal changes like lower levels of oestrogen can cause your blood pressure to rise.
- And some symptoms of menopause, like sleeping badly or feeling more stressed, can contribute to high blood pressure.
- But it’s important to remember that raised blood pressure is also a natural result of ageing – 30-50% of women experience high blood pressure before the age of 60.
What does this mean for you?
You don’t need to accept hypertension without action – there’s so much you can control and manage through lifestyle and wellbeing to not only reduce your blood pressure, but improve your overall health and longevity.

Does blood pressure fluctuate during menopause?
Yes – it’s common to see blood pressure readings fluctuate during menopause.
That can be caused by things like:
- Hormonal changes
- Stress
- Inconsistent sleep
It’s also possible for blood pressure to suddenly increase during menopause, so it’s useful to check your blood pressure regularly, even if previous readings were in the normal range.
And checking your blood pressure at home can give you a more accurate picture of your health.
Some people notice their blood pressure goes up when they’re feeling anxious, especially during medical appointments. This is sometimes called white coat syndrome.
What can you do?
Taking your blood pressure at home, where you’re more relaxed, can help you understand what your readings are like day-to-day.
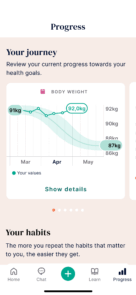
Tracking these readings over time can give you and your GP a clearer picture.
Apps are a great way to record and monitor your blood pressure – that’s why we’ve included it as a feature in the Oviva app.
Best practice would be to monitor blood pressure:
- 2-3 times weekly: track fluctuations while keeping things manageable.
- Daily readings can be helpful if you’re starting a new medication or have been advised to monitor more closely.
Ideally, measurements should be taken at the same time each day.

“During and after menopause, changes in hormones can affect blood pressure in ways that aren’t always obvious. It’s common to feel unsure about what’s normal, but even small changes to your eating habits, activity levels and daily routines can help support your heart health. There’s no one-size-fits-all approach, so it’s important to find what works for you.”
Lucy Diamond, registered dietitian
What blood pressure is normal during menopause?
Normal blood pressure is between 90/60 and 120/80 mmHg and the NHS uses the same blood pressure guidelines before and during menopause.
The chart below shows average blood pressure ranges for women over 40. These figures are based on population data, so they’re a guide – not a definition of what’s normal for everyone.
What’s most important is understanding your own pattern over time. If you’re noticing changes or have any concerns, it’s a good idea to speak to your GP.
| Age Group | Systolic (mmHg) | Diastolic (mmHg) |
| 40-59 | 112 | 74 |
| 60+ | 139 | 68 |
Source: The Heart Research Institute
- 140/90 or above if you’re under 80
- 150/90 or above if you’re over 80
How to manage high blood pressure during menopause
Managing high blood pressure during or after menopause isn’t about doing everything perfectly – it’s about finding small, realistic habits that work for you.
Here are some lifestyle changes you can make to help:

Movement that works for your body
You don’t need to run marathons or join a gym to support your heart health. What matters most is finding ways to move that feel doable and enjoyable.
Some great options include:
- Walking – a daily walk, even just around the block, can gently improve your circulation and help regulate blood pressure.
- Yoga or stretching – improve your strength and flexibility, while helping reduce stress hormones that raise blood pressure. Searching platforms like YouTube for “yoga for beginners” is a great place to start.
- Isometric training – research also shows that isometric training is great for reducing blood pressure. This is where you hold a position rather than moving through it, for example:
- A glute bridge
- Sitting against a wall in a chair-like pose
- Holding a lunge position
- Plank pose
A good routine for isometric training is to hold the position for five to 30 seconds, pause for one minute, then repeat for three rounds in total.
Tip: Start small and build from there. Even 5 minutes of movement counts.
Food choices that support your heart
There’s no perfect way to eat, but certain changes can support your blood pressure without feeling restrictive.
You could try:
- Adding more vegetables and whole grains – these are full of fibre, which helps keep your heart and digestive system healthy.
- Choosing lean proteins like fish, chicken, tofu or beans.
- Using less salt – try flavouring with herbs, lemon or garlic instead.
- Cutting back on processed foods which tend to have hidden salt and sugar, which can raise blood pressure.
Many people benefit from following a DASH diet which is based on these principles.
Tip: You don’t need to give up your favourite meals. Small, sustainable changes, like cooking one more meal at home each week, are a good place to start.
Making stress management more realistic
We understand that telling someone to “just relax” isn’t helpful. Stress is part of life, especially if you’re juggling work, family, health or finances.
Instead, think about what helps you feel more balanced. That might include:
- Saying no more often – protecting your time and energy can be an act of self-care.
- Breathing exercises – try inhaling for 4 seconds, holding for 4, and exhaling for 6. Just a few rounds can calm your nervous system.
- Doing something just for you – reading, music, stretching, even a moment of quiet. It doesn’t have to be big.
Tip: Stress affects blood pressure, but it’s not about being stress-free – it’s about finding moments of calm where you can.

Sleep support that works in real life
Sleep can be harder during menopause, especially with night sweats or anxiety. We know it’s not as simple as going to bed earlier – so here are a few things that might help over time:
- Keep a wind-down routine – something as simple as washing your face, brushing your teeth, and reading can signal to your body it’s time to rest.
- Dim the lights an hour before bed – light affects melatonin, the hormone that helps you sleep.
Use calming audio or white noise to help quiet your mind if thoughts are racing.
Tip: You don’t need perfect sleep every night. Even small improvements, like 20 more minutes of rest, can support your health.
Where weight loss can help
Extra weight, particularly around the middle, can raise your blood pressure and losing even a small amount of weight can help lower blood pressure. It can help you manage your menopausal symptoms too.
This isn’t about being restrictive, extreme dieting or big overnight changes that are hard to maintain. It’s about building realistic habits that support weight loss long term.
If you have a BMI over 35 and a weight-related health condition like high blood pressure, you may be eligible for NHS-funded support through Oviva. That includes:
- Personalised care from doctors, dietitians and psychologists
- Guidance around emotional eating, menopause and motivation
- Access to weight loss medications, if appropriate
- A tracking app to monitor blood pressure, food and goals

What I love about Oviva is that I can eat what I want — it was a completely new experience for me not to count calories. I lost 5 kg in the first 12 weeks, and my blood pressure normalised.
Can HRT cause high blood pressure?
Hormone replacement therapy is the most common medicine used to treat menopause, replacing hormones that are at lower levels. There are two main types of HRT: oral treatments, such as HRT tablets, and transdermal methods, which include gels, patches and sprays.
Research shows that oral HRT may increase systolic blood pressure. This occurs because oral HRT can raise angiotensinogen levels in the liver, leading to hypertension.
The same effect is not present with transdermal methods, which can often be used safely.

Can you take HRT if you have high blood pressure?
There are two main types of hormone replacement therapy (HRT):
- Oral HRT – usually taken as tablets
- Transdermal HRT – absorbed through the skin via gels, patches or sprays
Research suggests that oral HRT may raise systolic blood pressure in some people. This is because it can increase certain hormone levels in the liver (specifically angiotensinogen), which may lead to high blood pressure.
Transdermal HRT does not appear to have this effect, and is often considered a safer option for people concerned about blood pressure.
If you’ve been denied HRT due to hypertension, it can be frustrating and upsetting, but there may still be options available to you.
You may benefit from seeking out a specialist menopause clinic – you can find a list of the UK clinics here.
All clinics listed are recognised by the British Menopause Society (BMS). You can filter based on location and whether they’re NHS or private clinics.
Will high blood pressure stop when menopause is over?
For some people, blood pressure improves after menopause, especially with the right support. In many cases, it can stay slightly raised, due to natural hormone shifts and the effects of ageing on blood vessels.
That doesn’t mean it’s out of your hands. Regular monitoring and the small, realistic lifestyle changes we’ve recommended can make a meaningful difference to your blood pressure and overall heart health.

Take control of your health – one step at a time
If you’re living in England, have a BMI over 35 and a weight-related health condition like high blood pressure, you may be eligible for NHS-funded weight loss support with Oviva.
With Oviva, you’ll receive:
- Personalised care from a team of dietitians, doctors and psychologists
- Access to the Oviva app, where you can log meals and activity, track your blood pressure, set goals and monitor progress
- A flexible, realistic approach to weight loss – no calorie counting, no crash diets
- If appropriate, access to prescription weight loss medication
Our goal is to help you feel more in control of your health, at your own pace.