Can insulin resistance cause weight gain? And how to manage it
Insulin resistance occurs when your body’s cells don’t respond as well to insulin, whether it’s the insulin you naturally produce or the medical insulin you take. This means that insulin resistance can lead to weight gain. However, insulin resistance can also be caused by excess weight.
We take a closer look at how to lose weight with insulin resistance and how the support of a weight management programme like Oviva’s can help you.
Key Takeaways
- Insulin resistance can be caused by genetic factors (like PCOS or family history) and lifestyle factors (like being overweight or inactive).
- Symptoms include blood glucose changes and a slowing of the metabolism – both can cause weight gain.
- Insulin resistance can be caused by excess weight and can also cause weight gain, creating a loop.
- Oviva can help you manage insulin resistance and weight through professional, holistic support and lifestyle interventions.
What is insulin and what does it do in the body?
Insulin is a hormone that your body makes in the pancreas. When you eat, your body breaks down food into glucose (sugar), which enters your bloodstream.
Insulin helps move this glucose from the bloodstream into your cells, where it can be used for energy.
Think of insulin like a “key” that unlocks the door to your cells so they can absorb glucose.

What is insulin resistance?
When you develop insulin resistance, your cells (like those in muscles, fat, and the liver) become less sensitive to insulin. This means the “key” (insulin) isn’t unlocking the door to the cells as well as it should. So, even though you have insulin in the blood, it’s not working as effectively.
As a result:
- The glucose stays in the blood instead of being taken into the cells.
- Blood glucose levels rise because the glucose isn’t being processed and absorbed into cells.
Your body produces more insulin than usual to try and get your cells to absorb glucose, but your cells are still resisting that insulin. So, as well as high blood glucose, you have higher insulin levels.
How do you know if you have insulin resistance?
If you have insulin resistance, you may not have any symptoms early on. However, over time, it can cause changes in your blood glucose, and you may start to experience:
- Tiredness
- Hunger and cravings
- High blood pressure
- Skin changes
- Brain fog
- Weight gain, especially around the belly
Some of these symptoms can indicate other health conditions, too, so it’s essential to speak to a doctor.
A family history of insulin resistance or associated conditions, such as polycystic ovary syndrome (PCOS), pre-diabetes or type 2 diabetes, can also help to indicate that these symptoms are being caused by insulin resistance rather than another health condition.
There are also lifestyle risks, including weight gain and a lack of physical activity. If you have gained weight, these symptoms may be more likely to stem from insulin resistance.
If you think you may have insulin resistance, speak to your GP. It can be diagnosed by combining physical examination, blood tests, blood pressure checks and glucose testing.

Does insulin resistance cause weight gain?
Insulin resistance makes your cells less sensitive to insulin. So, when you eat, it becomes harder for glucose to be removed from your bloodstream and into your cells to provide energy.
This can elevate blood glucose levels. When your body has excess glucose not being used for energy, it stores this as fat, often around the midsection. This is significant because excess fat around the midsection is a risk factor for cardiovascular disease.
Then, your pancreas produces more insulin to try to compensate for this increase in blood glucose. As a result, overall insulin levels in the body increase, as well.
Multiple studies show that elevated insulin levels can cause weight gain. This is partly because insulin acts as a growth hormone, and elevated growth hormone levels can make you feel hungry, which means you’re likely to eat more than your body needs.
Insulin resistance can also lead to blood glucose crashes, which can cause you to crave more high-carb and high-sugar foods as your body seeks a quick energy boost. These blood glucose crashes happen because your body produces more and more insulin, and eventually, too much glucose is taken out of the blood and into your cells.
At the same time, when your cells struggle to absorb glucose for energy, your body thinks it is in a low-energy state. It responds by slowing your metabolic rate to conserve energy, reducing the number of calories you burn and encouraging your body to store more fat.
Can I still lose weight with insulin resistance?
Weight loss and insulin resistance have a complex relationship because weight loss can improve the symptoms of insulin resistance, but insulin resistance makes weight loss more challenging. However, with the right lifestyle changes and support, you can lose weight with insulin resistance.

Focus on a balanced, low-glycaemic diet
Try to eat a diet based on low-glycaemic index (GI) foods.
The glycaemic index ranks foods on a scale of 0 to 100, based on the rate at which the energy they provide is broken down into glucose.
Low-GI foods are broken down more slowly, meaning they release glucose gradually into the bloodstream rather than causing a rapid spike. This helps your blood glucose levels stabilise, as insulin resistance can lead to high blood glucose levels.
Foods are considered “low-GI” if they have a score under 55 on the glycaemic index. They include vegetables, whole grains, legumes and nuts like:
- Broccoli
- Cabbage
- Lettuce
- Kidney beans
- Lentils
- Chickpeas
- Quinoa
- Apples
- Berries
- Almonds
- Hazelnuts
As part of your balanced diet, you should also try to eat healthy fats found in nuts, avocado, and olive oil, and ensure you’re consuming sufficient lean protein found in chicken, fish, tofu, and eggs. This will help you to feel full and reduce cravings.
Avoid processed carbs and foods high in sugar, as they have a high GI and can cause insulin spikes. This is because these foods break down quickly into simple sugars, rapidly raising your blood glucose levels. In response, your body produces more insulin to move this glucose into your cells.
Exercise regularly
Aerobic exercise helps your body use insulin efficiently. That’s because when you do aerobic exercise, your muscles need more energy, so they pull glucose from your bloodstream to fuel movement. Normally, insulin helps glucose enter cells, but muscle contractions during exercise activate a separate pathway that allows glucose to enter without relying on insulin.
So your muscles become more efficient at using glucose, reducing the amount of insulin needed to keep blood sugar levels stable.
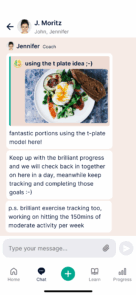
Aerobic exercise is any exercise that increases your heart rate and breathing rate for a significant time. Examples include brisk walking, swimming and cycling. The NHS recommends 150 minutes of moderate-intensity exercise per week.
Strength training also builds muscle, which can improve insulin sensitivity. Increases in muscle mass improves the number of glucose receptors in your muscles, allowing them to store and use more glucose, improving long-term blood sugar control.
Muscle tissue also burns more calories than fat tissue. Over time, strength training can help alter your body composition to improve your metabolism.
And if you’re losing weight, strength training is important to minimise the loss of any muscle mass.

Control portion sizes
Insulin resistance can slow your metabolism because your body becomes less efficient at turning glucose into energy. Therefore, controlling your portion sizes is crucial to avoid weight gain. Even healthy foods can cause weight gain if eaten in large quantities.
Here are some tips for controlling portion sizes:
- A smaller plate makes portions look bigger, tricking your brain into feeling more satisfied.
- Instead of eating straight from the pan or keeping serving dishes on the table, plate your meal first to prevent mindless second helpings.
- Vegetables are high in fibre and water, making them filling while keeping calorie intake low.
- Eat slowly and chew thoroughly – it takes about 20 minutes for your brain to register fullness.
- Drink water before and during meals as thirst can be mistaken for hunger.
- Avoid distractions when you’re eating like watching TV or scrolling on your phone – you’re more likely to notice when you feel full.
Time your meals wisely
It’s important to avoid skipping meals, as this can lead to blood glucose crashes. This, in turn, can make you more likely to overeat later, resulting in weight gain or a weight loss plateau.
Some people benefit from time-restricted eating, or intermittent fasting, which means you eat within a 10-12 hour window and avoid food outside of this window. Studies on the benefits of intermittent fasting are mixed but it may help to regulate insulin levels.
Medical support
If you’re struggling to lose weight with insulin resistance, it may be beneficial to seek medical support. Your doctor may be able to help you manage weight loss and insulin resistance.
You may also benefit from medications like metformin or GLP-1 receptor agonists like Wegovy. If you’re eligible, your doctor may refer you to a weight management programme, such as Oviva, through which you could receive prescription weight loss medication.

Manage stress and sleep
Stress and poor sleep quality can worsen insulin resistance and may also increase the effects of hormones like cortisol, which stimulates appetite.
You should aim to get 7-9 hours of quality sleep each night. You may be able to reduce stress by making changes to your lifestyle, increasing exercise and adopting some evidence-based stress-management techniques, including meditation, breathing exercises and yoga.
Track your progress
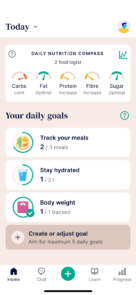
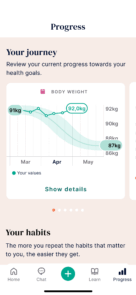
Use a food diary or tracking app to monitor your food intake and physical activity levels. Set small, realistic and measurable goals to help you stay motivated on your weight loss journey.
The Oviva app provides options for tracking your meals, exercise, mood and weight so you can see your progress over time and receive personalised feedback from your coaches.

Can insulin resistance be reversed?
Yes, with positive lifestyle changes and consistent behaviour, you can reduce the effects of insulin resistance and improve insulin sensitivity. This includes adopting a healthy diet and getting plenty of exercise. Using metformin and weight loss medications can also help.
It’s also important to understand that insulin resistance can be a precursor to type 2 diabetes. Early intervention through lifestyle changes can prevent the progression of diabetes. If your insulin resistance progresses, you can also potentially reverse type 2 diabetes.
We can support your weight loss journey
If you’re living in England, have a BMI over 35 and have relevant comorbidities, including PCOS, type 2 diabetes, asthma, depression or acid reflux, you could be eligible for Oviva’s Tier 3 Weight Management programme. You’ll receive multidisciplinary support from dietitians, doctors, and psychologists and could be able to access prescription weight loss medication.
As part of the programme, you’ll receive personalised care and support, access to a mobile app to track your progress, and the ability to learn how to make sustainable changes to your lifestyle.
97% of Oviva users would recommend us to others. Oviva users lose an average of 13.6 kg in the first 12 months.
It’s easy to get started – book an appointment with your GP and ask them to check if you’re eligible.
If you are, they can refer you to us quick and easy!
Want some help starting the conversation with your doctor? Just take our handy info pack to your appointment.