Understanding depression and weight gain: the relationship between mental health and obesity
The connection between depression and weight gain is complex. If you’re experiencing both, you’re not alone. There are small, manageable actions you can take to feel more in control, and speaking to your GP can be a helpful first step.
If you need urgent mental health support, call 999 or 116 123 for Samaritans.
If you’ve been struggling to lose weight for a while and have a BMI over 35, Oviva’s NHS-funded weight management programme could help. It gives you structured support to build healthier habits for your long-term wellbeing. It’s completely personalised to you and 100% remote.
Key Takeaways
- Depression and weight gain are linked through psychological, biological, behavioural, and medical factors. It’s common to notice weight changes when experiencing depression or persistent low mood.
- The relationship is cyclical – one can lead to the other. Your GP can help you understand the root cause and explore support options.
- Oviva’s weight management service offers evidence-based support to make sustainable lifestyle changes, but Oviva is not a mental health service.
- If you need mental health support, you can speak to your GP or contact your local NHS Talking Therapies Service. For urgent support, call 999.

Table of Contents
Understanding depression and feelings around weight gain
The relationship between depression and weight gain
The cycle of depression and obesity
Differentiating between physical and emotional drivers of weight gain
What can help with managing weight gain alongside low mood or depression?
Understanding depression and feelings around weight gain
Depression is a mental health condition and can feel like continuous low mood, sadness, or low self-esteem. You may also experience:
- A lack of motivation or interest in things you usually enjoy
- Feelings of irritability, anxiety, or guilt
- Difficulty concentrating or disrupted sleep patterns
It’s normal to feel sad at times, but depression is ongoing and can start to affect your work, family, or social life. It can also build gradually, making it hard to recognise when it started or how it differs from day-to-day low mood.
If you’re experiencing persistent low mood or think you may be depressed, speak to your GP. You don’t have to wait until things feel severe or meet every symptom to ask for help. If you need urgent support, call NHS 111.
Reaching out can be a positive first step, and support is available to help you feel more in control.
The relationship between depression and weight gain
Different factors can contribute to the relationship between depression and weight gain. Understanding these factors may help you make sense of your own experience.
Pay attention and consider jotting down the factors below that ring true for you. This can be really useful information to share with your GP.

Biological and hormonal factors
Depression is linked to chronic stress, which can lead to elevated cortisol levels or a cortisol imbalance.
- Cortisol and weight gain – Research suggests that high cortisol levels can stimulate appetite and increase fat storage, particularly around the abdomen. Elevated cortisol is also linked to insulin resistance, which may contribute to weight gain.
- Hunger hormones – Depression can disrupt the balance of leptin and ghrelin, the hormones that regulate hunger and fullness. This may cause you to feel hungrier than usual or less satisfied after meals.
- Serotonin and cravings – Serotonin, the hormone that helps regulate mood, is often lower in people experiencing depression. When serotonin levels drop, your body may crave foods that provide a temporary mood boost, such as refined carbohydrates and sugars.
If you’ve noticed you’re craving more sugary foods than usual, adding a few healthy snacks to your food cupboard may be helpful. Try to choose foods you genuinely enjoy, whether a few squares of dark chocolate or some Greek yoghurt with berries. This way, you can reach for these healthy snacks when your cravings hit and avoid less healthy options.
Medication side effects
When exploring the link between depression and weight gain, it’s also important to consider the potential side effects of medication.
Some antidepressants are associated with weight gain, and you may notice changes in your appetite, metabolism, or how your body stores fat.
Always prioritise your mental health, and don’t avoid antidepressants that may help you. It’s possible to lose weight while taking these antidepressants, and weight gain is not inevitable. By taking small steps, you can build healthy habits that help you to manage your weight.
If you’re concerned about weight gain related to medication, speak to your GP. They can help you understand your options and explore any possible adjustments to your treatment plan.
Sleep disturbances
Depression can affect sleep in different ways, causing some people to sleep less and others to sleep more than usual. These changes can disrupt circadian rhythms, which may affect fat storage and appetite regulation.
Poor sleep quality can also increase cravings for high-calorie or sugary foods, while a lack of sleep may lead to fatigue. This can make it harder to stay active, which over time, may contribute to weight gain.
There are some small adjustments that may help improve sleep quality:
- Gentle movement during the day can support better rest at night.
- Keeping a regular sleep schedule may help regulate your body’s rhythms.
- Allowing time to unwind before bed, such as reading or reducing screen time, could make falling asleep easier.
If sleep problems are affecting your daily life, speaking to your GP may help.
Changing relationships with food
Depression can change the way you eat, though this looks different for everyone. You may notice:
- Increased appetite or cravings for calorie-dense foods that provide short-term comfort.
- Irregular eating patterns, influenced by changes in mood, concentration, or sleep. Some people experience binge eating on certain days, followed by low appetite on others.
- Less motivation to cook, which may lead to relying more on takeaways, fast food, or ready meals.
If you’re finding it hard to cook or make food choices that support your health, having convenient, nourishing options at home may help. Consider keeping foods you genuinely enjoy on hand, so they’re easier to reach for when cravings hit.
Behavioural changes
Depression can affect daily routines, leading to changes in activity levels and eating habits. You may find that:
- Spending more time in bed or being inactive means your body uses less energy throughout the day.
- Feeling less social may result in spending more time at home, where you might be more likely to snack or eat for comfort.
These changes can happen gradually and may be difficult to recognise at first. If you’ve noticed a shift in your routine, taking small, manageable steps – such as adding gentle movement or planning meals in advance – may help you feel more in control.
If low mood is affecting your daily life, speaking to your GP can be a helpful first step.

The cycle of depression and obesity
The link between depression and weight gain is often cyclical, meaning one can reinforce the other.
- Depression can lead to weight gain, as changes in appetite, activity levels, and motivation affect daily habits.
- Weight gain can contribute to depression, sometimes due to self-image concerns, feelings of frustration, or societal pressures.
- Physical symptoms linked to weight gain, such as joint pain, fatigue, or reduced mobility, may make it harder to stay active, which can further impact mood.
- Social withdrawal may increase, as depression and weight gain can both contribute to reduced confidence and less interaction with others.
If you’re stuck in this cycle, it’s understandable to feel frustrated or unsure where to start. There’s no right way to move forward – it might help to focus on what feels most manageable, whether that’s eating something nourishing, spending time outside, or speaking to someone you trust. If you feel ready, your GP can talk through support options with you.
Differentiating between physical and emotional drivers of weight gain
Depression and weight gain can be influenced by physical and emotional factors, which may need to be managed in different ways.
Physical drivers
These are biological factors that affect appetite, metabolism, and how your body stores energy. They include:
- Hormonal changes – Shifts in cortisol, leptin, and ghrelin levels can affect appetite and how your body processes food.
- Medication side effects – Some antidepressants can increase appetite or slow metabolism.
- Lower activity levels – Reduced movement due to fatigue or low mood can affect energy balance and metabolism.
Emotional drivers
Emotional eating – or ‘comfort eating’ – can be triggered by feelings of stress, sadness, or low mood. This may lead to:
- A preference for high-calorie foods that provide short-term relief but contribute to weight gain.
- Reduced motivation for exercise, leading to a more sedentary lifestyle.
- Disrupted sleep patterns, which can further impact appetite and energy levels.
Managing drivers
If you’re unsure what’s affecting your weight, a GP or medical weight management programme may be able to help.
What can help with managing weight gain alongside low mood or depression?
The fact that you’re reading this article is already an indicator that you want things to be different, and that’s an essential first step for managing weight gain and depression or low mood. The next step could be to seek professional help.
Talking to a mental health professional
Depression and weight gain can both feel stigmatising and asking for help can feel hard. It’s normal to feel this way, but speaking to your GP can be a significant first step.
You can ask for a referral for talking therapy. In England, anyone can self-refer to their local NHS Talking Therapy service.
You may want to go private. There are online and in-person options available across the UK.
You can also speak to your doctor about whether medications like antidepressants could be helpful. It’s OK to explore the different options before making a decision.
If you’re feeling overwhelmed or struggling with thoughts of self-harm or suicide, help is always available. You can call 111 and select the mental health option to speak to someone who can provide assistance or advice, or you can reach out to your GP for an urgent appointment.
If you need emergency help, please call 999.
You may also find it beneficial to speak to a free listening service:
- Call Samaritans on 116 123 or email jo@samaritans.org. You can call 24 hours a day, 7 days a week. Email responses may take several days.
- Text Shout Crisis Text Line by texting “SHOUT” to 85258.
- Call Mind on 0300 123 3393 or text 86463. This is not a crisis service – it’s a safe space to discuss your mental health. The helpline is from 9 am to 6 pm weekdays, except for bank holidays.
Support losing weight
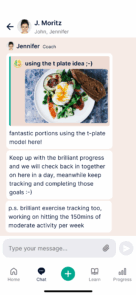
Losing weight alone can be hard. Having a team and community behind you, backing you all the way, can help you on your journey.
NHS-funded programmes like Oviva include support from a dedicated health coach, as well as guidance from dietitians, doctors and more. The right support can make lasting change.
Please note that while our team of psychologists can help you develop strategies for emotional eating and implementing behavioural change, Oviva is not a mental health service. We would always encourage you to contact your GP or call 111 for support.
Small habits add up
If you feel able, making small, gradual changes to your routine can help you take action at a pace that works. This can have benefits for your physical and mental wellbeing.
- Adjusting your diet – If it feels manageable, try eating more whole foods, reducing processed foods, or cutting back on takeaways. Choosing healthier snacks you enjoy can also be helpful. You can just pick one from this list to get started.
- Moving in ways that feel comfortable – Light activity, such as walking, stretching, or yoga, may support both your mood and energy levels. Even small movements, like walking in the sun or moving around the house more, can make a difference. That might look like trying to go for a five to ten minute walk every other day.
- Building a support network – If possible, talking to trusted friends or family may help. You could also join a support group or look into weight management services for additional guidance.
These changes don’t have to happen all at once – start with whatever feels achievable right now. That might simply be writing down a type of movement you’d like to try when you feel up to it.
If you’re struggling to make changes on your own, speaking to your GP or exploring professional support could be a helpful next step.
Professional weight loss support
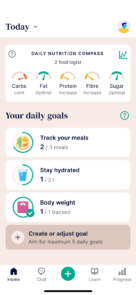
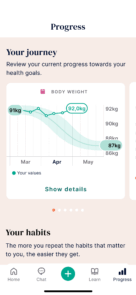
Oviva provides NHS-funded weight management support for eligible patients, offering personalised care that considers diet, medication, and behavioural support.
Our team of experts will work with you to set realistic goals and create a tailored action plan that supports long-term, sustainable change.
With Oviva, you’ll have access to:
- Support from dietitians, doctors, and psychologists
- The Oviva app to track your progress and stay connected to your support team
- The option to receive prescription weight loss medication, if eligible
Oviva’s service is free through the NHS, but eligibility depends on your location in England and certain criteria, including a BMI over 35 and at least one weight-related health condition, such as depression or type 2 diabetes.
Oviva’s psychology team can support you with behavioural change and emotional eating, but we are not a mental health service. If you need urgent mental health support, please speak to your GP or call 111. You can also self-refer to your local NHS Talking Therapy service.