The relationship between diabetes and weight gain
The link between weight and diabetes goes both ways. While carrying excess weight increases the risk of type 2 diabetes, diabetes itself can also make weight management more challenging. Insulin resistance, blood glucose fluctuations, and some medications may contribute to weight gain.
But you’re not alone – small, sustainable changes can make a real difference. And the right support can make managing weight with diabetes more straightforward. If you have a BMI over 35, you may be eligible for Oviva’s NHS-funded programme, which provides personalised weight loss support and access to weight loss injections.
Key Takeaways
- Both type 1 and type 2 diabetes can lead to weight gain in different ways.
- Type 2 diabetes is often linked to insulin resistance, which can lead to visceral fat around the midsection. This type of fat can increase health risks, but small changes can help.
- Managing weight with diabetes is possible. Small changes to eating, movement, and professional support can make a big difference.
- If you’re living with diabetes and excess weight, weight loss medication may also help by reducing hunger and supporting your efforts.
How diabetes can lead to weight gain
Can diabetes cause weight gain, and what is the nature of this relationship? Here, we’ll examine the links between type 1 or type 2 diabetes and weight gain.

Type 1 diabetes
If you have type 1 diabetes, your body does not produce insulin, but insulin is needed to convert food into energy. Without it, your body may break down fat and muscle for energy, leading to initial weight loss.
Why does insulin treatment lead to weight gain?
Once you start insulin treatment, you may notice some weight gain. This is:
- A normal part of recovery – as your blood glucose stabilises, your body can process food more effectively.
- Linked to insulin’s role as a growth hormone, which can naturally promote weight gain.
- Influenced by appetite changes – better blood glucose control can increase appetite.
Managing weight with type 1 diabetes
- Weight gain after starting insulin can be managed over time.
- Lifestyle changes, including balanced eating and physical activity, can help.
- Your diabetes team can support you in adjusting your insulin treatment and doses.
Type 2 diabetes
If you have type 2 diabetes, you may also have insulin resistance. This means your body doesn’t respond properly to insulin, whether it’s produced naturally or taken as medication.
Insulin’s job is to move glucose from your blood into your cells for energy. If you have insulin resistance, your body is making insulin, but your cells aren’t responding to it properly – this resistance causes problems.
Here’s how it leads to weight gain:
- Your body makes more insulin to compensate – Since your cells aren’t responding well, your pancreas releases even more insulin to try to get glucose into your cells.
- Insulin encourages fat storage – One of insulin’s roles is to store extra glucose as fat. The more insulin your body produces, the more fat it stores—especially around your midsection.
- Blood glucose spikes and crashes increase hunger – Because your cells struggle to absorb glucose, it stays in your blood, causing high blood glucose levels after meals. Your body then releases a lot of insulin at once to bring levels down. This can cause a blood glucose crash, making you feel tired, shaky, and hungry—often craving quick-energy foods like carbs and sugar.
- Your metabolism slows down – When cells struggle to absorb glucose, your body thinks it’s low on energy. In response, it stores more fat and burns fewer calories, making weight gain more likely.

How can I stop this cycle?
- Balanced eating – Choosing foods that keep blood glucose stable, like protein, fibre, and healthy fats, can help lower insulin levels.
- Moving more – Exercise makes your cells more sensitive to insulin, so they can absorb glucose better.
- The right support – A weight management programme can help you make these changes in a way that works for you.
With small, consistent changes, you can reduce insulin resistance and make weight loss easier. You’re not alone, and there are steps you can take to regain control of your health.
How does insulin resistance cause weight gain?
- The body produces more insulin to compensate for the insulin resistance.
- Higher insulin levels encourage fat storage, especially around the midsection.
- This can create a cycle where insulin resistance leads to more weight gain, making it harder to manage blood glucose levels.
- Blood glucose spikes and crashes can increase hunger and cravings, making it harder to maintain a balanced diet.
Breaking the cycle
- Lifestyle changes – eating a balanced diet and increasing activity levels can improve insulin sensitivity and stabilise blood glucose.
- Weight management support – the right guidance can help you reduce insulin resistance and maintain a healthy weight.
Even small, sustainable changes can make a big difference. With the right support, managing weight with type 2 diabetes is achievable.

The role of insulin and blood glucose
Insulin resistance and hunger signals
Insulin helps regulate hunger and feelings of fullness after eating. However, in people with insulin resistance, the brain may not respond as well to these signals. This can lead to:
- Increased hunger – making it harder to stop eating when full.
- More frequent overeating – which can contribute to weight gain.
- Blood glucose spikes and crashes
When insulin levels are out of balance, blood glucose can rise and fall quickly, causing:
- Sudden hunger and cravings for high-carb, high-sugar foods.
- Energy crashes, making you feel sluggish and craving quick fixes.
Hypoglycaemia (low blood glucose) and weight gain
Some diabetes medications can lead to hypoglycaemia (dangerously low blood glucose), which may require:
- Unplanned carbohydrate intake to stabilise blood glucose.
- Extra calories, making weight loss more challenging.
Even people not at risk of hypoglycaemia may fear it and eat unnecessarily, which can contribute to weight gain. If you’re unsure how to manage this, speak with your healthcare provider for guidance.
Diabetes medication and weight gain
Some diabetes medications can contribute to weight gain, but it’s still possible to manage your weight while taking them. And it’s essential to prioritise your diabetes treatment. If you’re concerned, talk to your doctor—they can help you find the most suitable treatment for your needs.
If you have type 1 diabetes, you’ll take insulin as a medication. Weight gain may occur as your blood glucose control improves.
Insulin is a possible treatment for type 2 diabetes and it can cause weight gain through:
- Increased fat storage – Insulin helps store excess glucose as fat, especially around the midsection.
- Increased appetite – As a growth hormone, insulin can stimulate hunger.
- Eating more due to hypoglycaemia – If blood glucose drops too low, extra food may be needed to stabilise it.
Sulfonylureas, a common diabetes medication, can also cause weight gain. Here’s how:
- They stimulate the production of insulin from the pancreas.
- This extra insulin helps to convert blood glucose from food into energy for your body.
- If the dose is too high, which can be challenging to assess initially, it can cause your blood glucose levels to fall too far.
- You may need to eat more to avoid hypoglycaemia, while low blood glucose can also increase your hunger levels.
How lifestyle factors make a difference
Diabetes can make it harder to maintain certain lifestyle habits, which can affect weight management.
- Energy levels and movement – Insulin imbalances can affect how well your body converts food into energy. This can leave you feeling low on energy, making exercise feel harder. But even small increases in activity—like short walks or stretching—can make a difference.
- Food choices – What you eat plays a key role in weight management. A balanced, nutrient-rich diet with plenty of fibre and protein can help, while reducing refined carbohydrates may support blood glucose control.
Focusing on small, achievable changes can help you feel more in control of your health.
Does diabetes cause belly fat?
Visceral fat—fat stored around the midsection and internal organs—can be harmful to your health. It’s linked to a higher risk of conditions like heart disease, stroke, and type 2 diabetes.
If you have type 2 diabetes and insulin resistance, your body may produce more insulin to manage blood glucose levels. Higher insulin levels can signal fat cells to store more glucose as fat, particularly around the abdomen.
Excess abdominal fat can also increase inflammation, which may further impact health. This is why managing weight and blood glucose levels together can be beneficial for overall well-being.
Is it hard to lose weight with diabetes?
Diabetes can make weight loss more challenging due to insulin resistance, blood glucose fluctuations, and certain medications. However, with the right approach, it’s absolutely possible—and losing weight can even help improve insulin resistance and diabetes symptoms.
Weight loss can also lower health risks like high blood pressure and cholesterol. Since diabetes adds extra challenges, it’s important to be kind to yourself and focus on sustainable changes rather than quick fixes.
A balanced approach—including nutritious eating, movement, and stress management—can make a real difference. If you’d like expert guidance, Oviva’s team of dietitians, doctors, and psychologists are here to support you.

Managing weight with diabetes
Making small, sustainable changes to your lifestyle can help with weight management while living with diabetes. Here are some key areas to focus on:
- Food choices
- Reduce refined carbohydrates and focus on lean proteins, healthy fats, and fibre-rich foods.
- Choose low-GI foods like vegetables, whole grains, and most fruits. Low-GI foods are foods that release energy more slowly, which helps prevent blood glucose spikes.
- Physical activity
- Exercise improves insulin sensitivity and helps with weight management.
- Try a mix of aerobic exercise (like walking, swimming, or cycling) and strength training.
- Stress management
- High stress can heighten cortisol levels which can increase appetite and slow metabolism.
- This makes you more likely to overeat and reduces the number of calories your body burns at rest.
- Reduce stress with good sleep, meditation, yoga, or aerobic exercise, which releases mood-boosting endorphins.

- Medications
- GLP-1 receptor agonists may help by reducing appetite and improving insulin sensitivity—speak to your GP to see if this is an option for you.
- If you often need to eat to prevent low blood glucose, ask your healthcare provider about adjusting your diabetes medication.
Medications can complement your lifestyle changes but should not be used in place of broader lifestyle changes. You should always be under medical supervision when taking weight loss injections like Wegovy and Mounjaro.
If you find you need to eat to prevent your blood glucose levels from dipping too low, discuss this with your healthcare provider and request a review of your diabetes medication. There may be a more suitable medication that enables you to eat less.
Foods to avoid when you have diabetes
Being mindful of your food choices can help with blood glucose control and weight management. Here are some foods to reduce:
- Refined carbohydrates and high-sugar foods
If you’re living with diabetes, it’s essential to be more carb-aware, as all carbohydrates will push up blood glucose levels.
Limit foods that are high in sugar, including refined carbohydrates like white bread and pasta, as well as high-carbohydrate meals. These can cause blood glucose spikes and may contribute to weight gain.

- Sugary drinks
Soft drinks, fruit juices, and energy drinks can quickly raise blood glucose levels. Opt for water, herbal teas, or zero-sugar drinks instead.
- Processed foods
Where possible, move away from processed and ultra-processed foods and aim to eat more foods in their natural state or meals you prepare from scratch using fresh ingredients. With busy lifestyles, this isn’t always possible or straightforward – just do what you can, when you can. Here are some dietitian-approved meal ideas for a healthy diet plan to inspire you.
- High-fat and salty foods
While healthy fats (like those in oily fish, nuts, and avocado) are beneficial, limit unhealthy fats found in fried foods, cakes, and processed snacks. Try to find a healthier alternative. For example, if you have a sweet tooth, opt for dark chocolate rice crackers or some dark chocolate coated nuts. Reducing excess salt can also help support heart health.

How a weight loss programme can support your diabetes diagnosis
A weight loss programme, like the one offered by Oviva, can support your diabetes diagnosis and equip you with the knowledge and support needed to make lifestyle changes. You’ll learn to eat a more balanced diet and increase activity in a sustainable way.
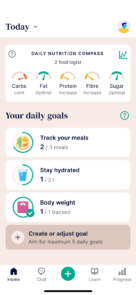
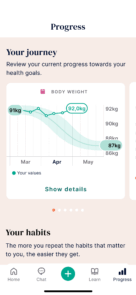
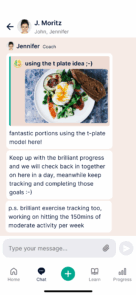
Oviva’s programme includes a smartphone app that offers tracking features. You’ll also communicate with expert coaches who can provide personalised advice.
Don’t take it from us. We are recommended by 97% of Oviva users.