How to lower cholesterol: simple steps that work
High cholesterol can increase your risk of heart disease and stroke, but there are practical, proven ways to lower your cholesterol. From making small tweaks to your diet to building sustainable habits around movement and alcohol, even small changes can add up to a healthier heart.
Oviva’s NHS-funded weight management programme is here to support you. If you have a BMI over 35 and high cholesterol, you may be eligible for personalised care – including expert guidance, behaviour-change support and, if appropriate, access to weight loss injections like Wegovy.
Key Takeaways
- Even a small amount of weight loss can help lower cholesterol by improving how your liver processes fats.
- Diet makes a difference – cutting back on saturated fats and eating more cholesterol-friendly foods like vegetables, beans and oats can help reduce levels.
- If your cholesterol is very high or runs in the family, you may need medication to help bring it down.
- Sustainable support works – a programme like Oviva can help you build healthy habits that last, with personalised guidance and behaviour change tools.
What is cholesterol, and why does it matter?
Cholesterol is a fatty substance made by your body and found in some foods. It plays an important role in keeping your cells healthy, but if your levels get too high, it can become a problem.
There are two main types of cholesterol to be aware of:
- HDL cholesterol – often called the ‘good’ cholesterol, as it helps remove excess cholesterol from your bloodstream.
- Non-HDL cholesterol – this includes LDL (‘bad’) cholesterol, which can build up in your arteries over time.
If your total or non-HDL cholesterol is too high, it can increase your risk of heart disease, heart attack and stroke.
Best lifestyle changes to lower cholesterol
Here are some evidence-based habits that can lower your cholesterol to support your heart health and lower your risk of serious conditions like heart disease and stroke.
1. Maintain a healthy weight
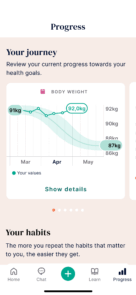
Losing even a small amount of weight can help lower your LDL (or ‘bad’) cholesterol and support heart health.
Try to aim for 5–10% of your body weight, and focus on gradual, sustainable changes.
- Start by reducing portion sizes
- Switch sugary drinks for zero-sugar options
- Cut back on fatty cuts of red meat and foods high in saturated fat
You don’t need to overhaul everything at once – each small change adds up.
Here are some simple, healthy habits you can do to lose weight.
2. Eat for heart health
Food plays a key role in managing cholesterol. The most helpful swaps are often the simplest.
- Eat more fibre: beans, lentils, oats, fruit, veg
- Swap saturated fats (like butter, fatty meat, full-fat cheese) for unsaturated fats (like olive oil, oily fish, almonds, and avocado)
- Try plant sterols and stanols: found in fortified spreads, yoghurts and milk, they’ve been shown to lower cholesterol when eaten regularly
Small swaps that you can stick to make a real difference to your cholesterol levels.
Some people wonder whether time-restricted eating or intermittent fasting could help reduce cholesterol.
Read more: Does fasting lower cholesterol?

3. Move more
Staying active supports healthy cholesterol levels and heart function.
Not sure where to start? Begin with what feels manageable – this could be a 2-minute stretch, a walk to the end of the street, or even seated movement at home.
The key is consistency, not intensity.
Small steps done regularly can build your confidence and stamina over time – what feels achievable today can grow into more movement tomorrow.
4. Quit smoking
Smoking can raise harmful cholesterol levels and increase your risk of heart disease and stroke.
If you’re thinking about quitting:
- Call the NHS Stop Smoking Service on 0300 123 1044
- Speak to your GP about support options
You don’t have to do it alone, and it’s never too late to quit.
5. Cut back on alcohol
Drinking alcohol regularly can raise your cholesterol, especially triglycerides, which increase the risk of heart disease.
If your cholesterol levels are high, reducing alcohol intake can help bring them down.
Try cutting back gradually, spacing out drinks, or switching to low- or no-alcohol options.

6. Get enough sleep
Your sleep habits can affect your cholesterol.
One study found that sleeping too little or too much was linked to lower HDL (‘good’) cholesterol and higher triglycerides.
If you’re not sleeping well, you’re not alone. Rather than focusing on a perfect number, start by building small habits that support better rest over time.
To support better sleep, try:
- Reducing screen time before bed
- Creating a quiet, dark sleeping space
- Introducing a wind-down routine, like gentle stretching or a warm drink
Even small improvements in sleep can have a positive effect on your overall health.
7. Manage stress
Stress alone doesn’t raise cholesterol, but the way we cope with stress can. Emotional eating, disrupted sleep, and less movement are all common responses that may affect your heart health.
You don’t need to overhaul your life to start feeling better. Instead, try building in small moments of calm that fit your routine.
Some ideas to explore:
- Gentle breathing exercises
- Spending time on a hobby you enjoy
- Taking a short break outdoors
The best stress management tools are the ones you’ll come back to. It’s not about getting it ‘right’, it’s about finding what helps and giving yourself permission to pause.

With Oviva, I feel truly supported.
Why weight loss is so effective for cholesterol
Carrying excess weight, especially around your middle, can increase cholesterol levels and contribute to insulin resistance. This type of fat, known as visceral fat, is also linked to inflammation in the body.
That matters because inflammation and high cholesterol together raise your risk of heart disease.
Losing weight can lower cholesterol, reduce inflammation, and support better metabolic health. It also reduces fat around the liver, helping your body process cholesterol more effectively.
- Aim for steady, sustainable weight loss – the NHS recommends around 1 to 2 lbs (0.5–1 kg) per week.
- Avoid quick fixes or crash diets. If faster weight loss is needed, make sure it’s done with professional support.
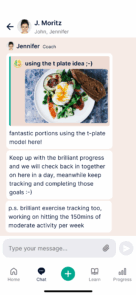
With Oviva’s NHS-funded programme, you’ll get expert guidance from dietitians, doctors and psychologists so you can build lasting habits that support heart health and cholesterol management.
How long does it take to lower cholesterol?
Lowering cholesterol through lifestyle changes and weight loss takes time, but small, consistent steps can lead to real progress.
You may start to see a difference in your cholesterol levels within four to six weeks, but more significant improvements often take several months.
That’s why it’s important to focus on sustainable changes you can stick to.
- Aim for consistency, not perfection.
- Be realistic about what you can change and give yourself credit for trying.
- If things don’t go to plan, it’s not failure. Show yourself compassion and return to your goals when you’re ready.
If you’re prescribed cholesterol-lowering medication, such as statins, you may notice a reduction in cholesterol within around four weeks, especially if you have a family history of high cholesterol.

When to see a doctor or try medication
Diet and lifestyle changes can help most people lower cholesterol, but they’re not always enough.
There’s no one-size-fits-all solution – if you’re struggling, speak to your GP about next steps.
Medication may be prescribed if:
- You have familial hypercholesterolaemia – high cholesterol with a genetic link
- Your cholesterol levels are very high and need to be brought down quickly
- You have an established history of heart disease
- You’re deemed to be at increased risk of heart disease
Statins are a common medication and can start to lower cholesterol in as little as four to six weeks.
If you’re prescribed medication, it’s important to follow up with your GP and have regular tests to track your progress.
Take control of your well-being with Oviva
If you have a BMI over 35, you may be eligible for Oviva’s NHS-funded weight management programme.
You’ll receive personalised care from registered UK dietitians and health coaches, with support to lower cholesterol and build lasting healthy habits.
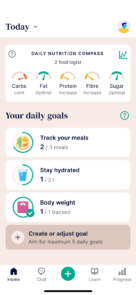
Through the Oviva app, you can:
- Message your coaching team and get tailored guidance
- Log meals, movement and weight to track your progress
- Access expert resources on nutrition and lifestyle
- Get real-time feedback on your meals and daily nutrient intake
If appropriate, you may also be eligible for prescription weight loss injections.