Type 2 diabetes: signs, treatments and lifestyle support
Type 2 diabetes develops gradually, and recognising the early signs—such as tiredness, increased thirst, frequent urination, and blurred vision—can help you take control of your health. If you have these symptoms, speaking to your GP is important for early diagnosis and management.
Treatment often includes medication and lifestyle changes. With the right support, weight loss can improve blood glucose levels and may even lead to remission, reducing the need for medication. Oviva’s personalised weight management programme is designed to help you achieve lasting, sustainable changes.
Key Takeaways
- Type 2 diabetes is a long-term health condition caused by the body not producing or not using insulin effectively. It can cause high blood glucose levels.
- Over time, too much glucose in the body can lead to some serious health complications, including heart disease, stroke and kidney issues.
- Type 2 diabetes treatments can include lifestyle changes to promote weight loss and diabetes medications that help to stabilise blood glucose levels.
- Remission is possible – with the right support, weight loss and lifestyle improvements can help you take control of your health and reduce the need for medication.
What is type 2 diabetes?
Type 2 diabetes is a long-term medical condition caused by insufficient insulin production or the body’s inability to use insulin effectively.
Insulin is a hormone that helps regulate blood glucose levels. When it isn’t functioning properly, glucose builds up in the bloodstream, leading to high blood glucose levels.
Over time, excess glucose can cause damage within the body and lead to serious complications, including heart disease, stroke, kidney problems, nerve damage, and vision loss.

Type 1 vs. type 2 diabetes: what’s the difference?
Diabetes is a chronic health condition that causes blood glucose levels to become elevated. However, it can be broken down into two types, with different characteristics and treatments:
- Type 1 diabetes: An autoimmune condition whereby the immune system destroys insulin-producing cells in the pancreas. Treatment requires daily insulin injections.
- Type 2 diabetes: Often linked to weight gain and insulin resistance and caused by lifestyle factors like being inactive, alongside genetic predisposition.
The pancreas initially compensates for insulin resistance by producing extra insulin but eventually cannot keep up, leading to rising blood glucose levels.
Treatment for type 2 diabetes involves lifestyle changes and, if needed, medication like Ozempic to help manage blood glucose levels.
Risk factors for type 2 diabetes
You may be at increased risk of type 2 diabetes if you:
- Are over 45 years old.
- Have a family history of diabetes.
- Have a sedentary lifestyle.
- Are overweight, especially around the abdomen.
- Have medical conditions such as polycystic ovary syndrome (PCOS), high blood pressure, or high cholesterol, or use certain medications, like steroids.
Your risk of developing type 2 diabetes may also be elevated if you experience gestational diabetes, which occurs when blood glucose spikes during pregnancy.

Symptoms of type 2 diabetes
Typical type 2 diabetes symptoms include:
- Frequent urination
- Excessive thirst
- Persistent fatigue
- Unexplained weight loss
- Blurred vision
- Slow-healing sores
Other signs can include tingling in the hands or feet, frequent infections, and dry, itchy skin. If you notice any of these, consult your doctor for a proper diagnosis.
How is type 2 diabetes diagnosed?
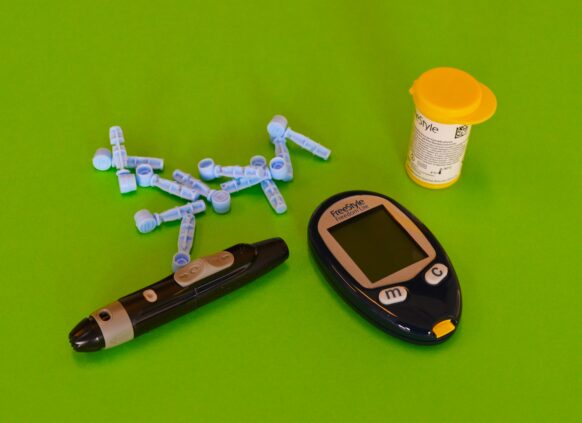
Type 2 diabetes can be diagnosed by your GP through blood tests, such as:
- Fasting blood glucose tests
- Oral glucose tolerance tests
- HbA1c tests (measuring average blood glucose levels over 2–3 months)
Early diagnosis is crucial for managing the condition effectively and preventing complications.
Treating and managing type 2 diabetes
Treatment focuses on controlling blood glucose levels and preventing complications through:

Lifestyle changes:
- Weight management: Losing excess weight can significantly improve blood glucose control. If you have type 2 diabetes and a BMI of 35+, you could access Oviva’s weight management programme for professional weight loss support.
- Regular physical activity: Aim for at least 150 minutes of moderate exercise per week, which can include brisk walking, riding a bike or mowing the lawn.
- Dietary adjustments: Incorporate vegetables, whole grains, lean proteins, and healthy fats. Avoid sugary drinks and processed foods. Increase awareness of carbohydrates and aim for a reduction in overall carb intake.
- Managing stress and lowering cortisol levels: In addition to using relaxation techniques, you can lower cortisol levels by eating a healthy diet and exercising.
- Staying hydrated: This is important because high blood glucose levels can increase the risk of dehydration.
- Getting enough sleep: Poor quality sleep can elevate blood glucose levels and worsen insulin resistance.
- Quitting smoking: People who smoke and have diabetes are more likely to have issues with diabetes management, including insulin dosing.
Medications:
- Metformin: A medication that lowers blood glucose levels by improving your body’s response to insulin. Usually prescribed if diet and exercise alone do not control diabetes symptoms.
- Sulfonylureas: A class of medications that increase insulin production in the pancreas. This can then lower blood glucose levels.
- Gliptins: A group of medications that help to preserve hormones called incretins, which reduce blood glucose after eating.
- Dapagliflozin: A medication that targets your kidney function, increasing the amount of glucose removed from the body when you urinate.
- Injectable options like insulin and GLP-1 medications, including Ozempic.

Monitoring:
- Regular blood glucose monitoring or periodic HbA1c tests help track progress.
These changes can all help to maintain stable blood glucose levels.
The role of weight management in type 2 diabetes
How does weight affect diabetes?
Excess weight, especially around the abdomen, increases insulin resistance, making it harder for the body to regulate blood glucose.
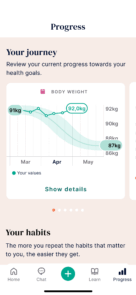
Losing weight, particularly after a recent diagnosis, can help manage type 2 diabetes and may even place the condition into remission.

Tips for managing weight with type 2 diabetes:
- Set realistic goals to achieve steady, sustainable weight loss.
- Watch portion sizes, keeping carbohydrates to a quarter of your plate.
- Become more active or at least reduce sedentary time.
- Focus on a balanced diet with plenty of vegetables, some fruit, lean proteins, and whole grains.
- Minimise unhealthy fats and opt for healthy options like olive oil.
- Celebrate small milestones and seek support from family, friends, or healthcare professionals.
Find out more about the relationship between diabetes and weight gain.
Living with type 2 diabetes
Living with type 2 diabetes requires daily care, but with the right tools and support, it’s manageable. Key steps include:
- Staying informed about your condition and treatment options. You should have check-ups with your doctor multiple times per year. New treatment options may also emerge, and the ideal treatment for you may depend on changes in your health and lifestyle.
- Developing a personalised treatment plan with your doctor. It’s crucial for this to be personalised because diabetes affects people differently – some people are able to manage their symptoms without medication, and some people have better results using one medication type than another.
- Joining support groups or accessing online resources to share experiences and stay motivated. This can help you to stay on track with improvements to your lifestyle.

Support systems and resources:
A strong support system of family, friends and healthcare professionals can help you:
- Stay accountable to your treatment goals.
- Manage daily tasks like meal planning and exercise.
- Provide emotional encouragement and practical help.
Family and friends can also benefit from learning about type 2 diabetes to better assist you in your journey.
Is type 2 diabetes remission possible?
It is possible to put your type 2 diabetes into remission, reducing the need for medication and lowering the risk of health complications like heart disease.
Your chances are highest within the first six years of diagnosis, but it’s never too late to make positive changes and take control of your health.
Read our article: Can you reverse type 2 diabetes?
The best way to achieve this is through sustainable weight loss. The closer you can get to losing 10-15% of your total body weight, the better your chances of achieving remission.
Keeping weight off is also crucial for maintaining your remission status, and it’s best to seek professional support, such as from Oviva, to achieve this safely and long-term.

Preventing type 2 diabetes
While you can’t eliminate all risks, you can reduce your chances of developing type 2 diabetes by:
- Eating a balanced diet rich in whole, unprocessed foods.
- Maintaining a healthy weight.
- Engaging in regular physical activity.
- Avoiding smoking and limiting alcohol consumption.
- Attending routine health check-ups.
Could weight loss help your type 2 diabetes?
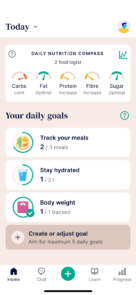
If you have type 2 diabetes and a BMI 35+, you could be eligible for Oviva’s weight management programme—designed to help you lose weight, improve blood glucose levels, and even achieve remission.
Here’s why thousands choose Oviva:
- Average weight loss of 13.6 kg in 12 months
- 97% of users recommend us
- Weight loss medication delivered to your door (if eligible)
- Expert-led support to help you keep the weight off for good
Find out if you’re eligible in two minutes.
Eligibility criteria varies based on your location in England.