
FOR people living with TYPE 2 DIABETES
NHS Type 2 Diabetes
Path to Remission Programme

About this programme
The NHS Type 2 Diabetes Pathway to Remission Programme (formerly NHS Low Calorie Diet Programme) provided by Oviva is an evidence-based intervention using Total Diet Replacement (TDR) to support people diagnosed with Type 2 diabetes to achieve significant weight loss (15kg), improvements in HbA1c, reduction in medication needs and potentially achieve diabetes remission.
Why should you refer your patients?
The programme supports patients to build sustainable self-management behaviours and drives long-term health improvements with support from healthcare professionals and effective learning resources.

Participants lost on average 14.7kg

Participants on average reduced their HbA1c by 33%

63% of participants achieved Type 2 diabetes remission
Programme pathway
The programme takes place over 12 months and is split into 3 stages. After 12 months, patients can continue to self-track their activities in the Oviva app and will have lifetime access to Learn resources.

Start
Participants will first have a consultation with a personal clinician who will help them prepare for the journey ahead. Together they’ll agree on goals for the programme, and come up with an action plan to help them achieve them over the 12 months.

Change
12 weeks on a low calorie diet using Total Diet Replacements products where they will replace all meals and snacks with shakes and/or soups. These contain all the essential vitamins and minerals needed. During this time, they will receive frequent support from their clinician. In the following 4 weeks, they will undergo food reintroduction with support.

Sustain
For the remaining eight months they will work on sustaining these healthy habits and will continue to have access to the Oviva app and learning resources. Find more about our digital tools here.
What’s the difference between digital and in-person coaching?

Complete flexibility
with no need for travel

Devices sent directly
to your home

Hassle free communication
so you can reply at any time
Eligibility criteria
There have been some recent changes to the eligibility criteria (December 2022), which can found by downloading the full eligibility criteria. The following referred patients can be accepted onto the programme:
- People aged between 18 and 65 years old
- People who are not pregnant
- Confirmed diagnosis of type 2 diabetes within the last 6 years
- Those who are motivated to change their lifestyle and can commit to the 12 month programme
- Registered in an area where Oviva is available

Referral information
How can primary care refer to the programme?
After confirming eligibility and discussing the service with your patient for the pathway please complete the referral form which is embedded into your clinical system and send it to: ovivauk.T2DR@nhs.net
Are there any resources to support primary care in referral conversations with patients?
Training Video
During this video, Caroline Hebberd, Service Manager at Oviva and Keren Miller, Diabetes Dietitian and Clinical Lead at Oviva explain the programme in more detail including the participant journey, the full eligibility criteria, how to refer and information on the referral form. We have two other videos available to you:
1. Medication Guidance
2. Short-form training video
Clinic locations
Updates

Searches
Searches are an efficient way to identify eligible patients for this programme. They ensure that all newly diagnosed patients are being flagged for referral, and that patients nearing the NHSE cut offs for age and date of diagnosis are referred before they fall outside of the eligibility criteria.
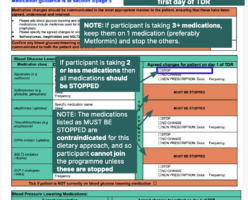
Medication adjustment information
Information on the medication adjustments that need to be made and communicated with patients can be found on the referral form. We have annotated the referral form so you can clearly interpret what needs to be actioned.

Medication changes information
Information on the medication changes that need to be made for your patients.







